Most brain tumours are only diagnosed after the patients start showing symptoms. There are a wide variety of medical examinations to diagnose a brain tumour. Normally, these different examinations are combined with each other.
Neurological Exam
The first step is to perform a neurological exam. The physicist will asses the patient’s symptoms by asking the personal and the family health history. This exam also includes: checking vision, hearing, strength, sensation, balance, coordination, reflexes, mental health and ability to think and remember [1]. Once the doctor suspects the presence of a tumor, the next step would be a scan of the patient’s brain.
There are different types of brain scans that may be used. They are useful to confirm intracranial abnormality, characterise the tumor and help to determine grade and make decision about biopsy.
Imaging Modalities
MRI (Magnetic Resonance Imaging)
-Spin Echo (SE) Sequences can be adjusted for T1, T2 or proton-density weighted images:
Case courtesy of A.Prof Frank Gaillard, <a href="https://radiopaedia.org/">Radiopaedia.org</a>. From the case <a href="https://radiopaedia.org/cases/21753">rID: 21753</a>
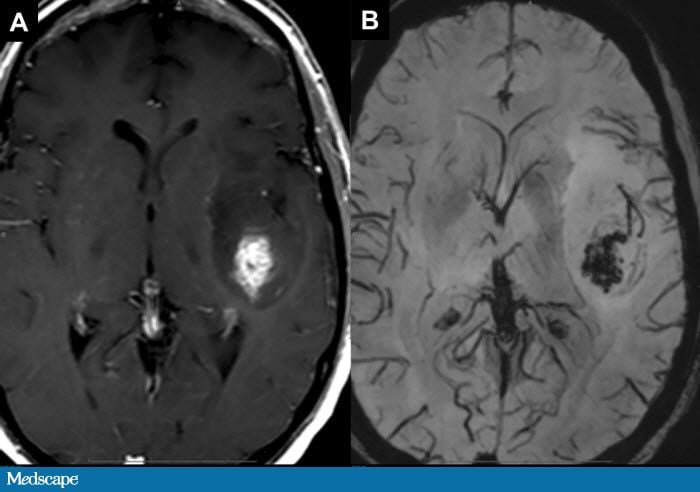
As SE Sequences tend to be long, faster techniques have been developed: Inversion Recovery Sequences and Gradient Echo Sequences, when a rephasing gradient is applied(for example Susceptibility Weighted Images, pictured below). This technique can also be used to suppress water (FLAIR) or fat signal.
A: T2 weighted and B: FLAIR Image of brain tumour. Source: http://www.medscape.org
- Properties of T1 weighted images: short repetition time(TR), long echo time(TE), fat tissue appears bright, and fluids appear dark
T2 weighted images, on the other hand, are obtained by applying a long TR and a long TE; fat appears as intermediate-bright, and fluid as bright[2]
Proton density weighted images: The higher the proton density the higher the intensity.
Examples of T1 weighted, T2 weighted and PD weighted MRI scans. Adapted with permission by Kieran Maher using Graphic Converter from [http://homepage.mac.com/kieranmaher/ait/ Applied Imaging Technology] by Heggie, Liddell & Maher (2000).
In order to improve the contrast in these images, Contrast Agents can be injected in the patient - the most widely used agent is Gadolinium III, and therefore it is possible to assess areas with higher metabolism.
Advantages and Disadvantages of the Method:
Pro:
no radiation, very good soft tissue contrast, resulting in more detailed images than in other types of scans.
Con:
availability, expense, distortion
Image source: [3]
CT(Computed Tomorgraphy)
Myelography
Myelography involves the introduction of a needle in the spinal canal to inject contrast material, and then evaluate the spread of this material around the spinal cord and the nerve roots through x-ray fluoroscopy. It can be used when MRI cannot be performed, or in addition to it, to retrieve information about the development or spread of a tumour to the spine, meninges, nerve roots or spinal cord. [6]
Cerebral Angiography
Cerebral Angiography is an imaging method that involves the investigation of blood vessels in the brain. There are 3 methods of carrying out this procedure:
- x-ray fluoroscopy with iodinated contrast agent
- CT with iodinated CA
- MRA (Magnetic Resonance Angiography), where the blood vessel signal is selected by special RF sequences [7],[8]
MRA Emphasising brain tumour. Image source: [9]
PET(Positron Emission Tomography)
PET(Positron Emission Tomography) is a nuclear imaging technique that assesses the metabolic process of the body. The images are obtained by injecting a gamma-emitting tracer in the human body and measuring the obtained radiation. The concentration of the tracer in the body can be reconstructing using 3D reconstruction techniques. The PET image will still have to be imposed over a regular MRI or CT image, in order to offer location information.
The most used tracer for tumor analysis is FDG( fludeoxyglucose ), as it is a “tagged sugar”, and sugar metabolism in tumours is increased. Informations can be obtained about metabolism, blood flow, oxygen consumption, amino acid metabolism, and lipid synthesis in tumours.[10]
PET scans are highly used in the evaluation of metastasis(90% of scans).
Disadvantages of the method are:
radiation, cost, resolution, registration
Image source: [11]
SPECT(Single Photon Emission Computerized Tomography)
Just like PET, SPECT can be used to obtain functional information about the brain. However, this method is more limited in the localisation of abnormalities.[12]
Dual SPECT/CT is often used for simplifying the registration of the images of the two modalities.
This information is useful for optimizing diagnosis, therapy monitoring, and radiotherapy treatment planning.
Source:[13]
MRS (Magnetic Resonance Spectroscopy)
Magnetic resonance spectroscopy (MRS) is a test using MRI that provides information on the chemical composition of the brain.
This technique helps determine the distribution of electrons around the nuclei. The base of this modality is the same as for MRI, but pulse sequences are used to cancel out the water signal, giving information about the chemical composition in the brain. [14]
Primary brain tumors show elevated choline and decreased NAA (N-acetyl aspartate) levels.
In the image on the right, we can see an MRS analysis of a Glioma.Image source: [15]
fMRI (Functional MRI)
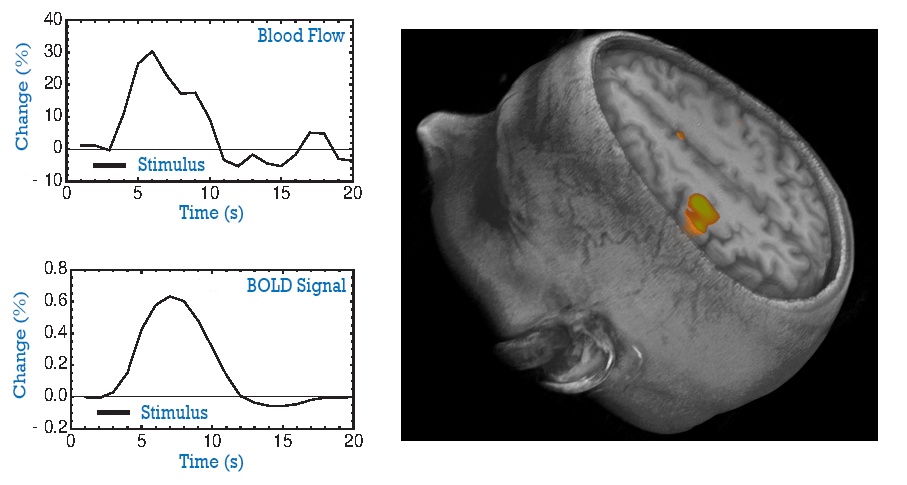
A functional MRI (fMRI) is a non-invasive imaging method that provides information about the activity of the brain. During the examination, the patient is asked to carry out certain tasks , and a change in brain activity will result in a slight (1%) change in the MRI signal emitted. [16] During the fMRI examination, the patient is asked to do certain tasks that cause changes in the brain and can be seen on the fMRI image. The reason for this signal is the fact that brain activity changes the level of blood oxygen in the activated areas. Oxygenated blood has a different T2 relaxation time than oxygen-poor blood, resulting in differences in 2 subsequent images, one taken with a stimulus, and one without. (This method is the bases of BOLD fMRI Tests).
Another fMRI technique is Arterial Spin Labeling (ASL), which works by manipulating the MR signal of the blood delivered to the brain. A control image and an tagged image are then acquired; subtracting these results in an absolute image, caused by the manipulated arterial blood.
Tumours can change the blood flow of the brain in ways that are not related to neural activity.This test is used to help plan surgery, so the surgeon can avoid damaging the functional parts of the brain while removing the tumor.
Courtesy of Dr Richard Buxton, UC San Diego
DWI (Diffusion Weighted Imaging)
Diffusion weighted imaging (DWI) is a form of MR imaging that relies on measuring the diffusion (random Brownian motion) of the molecules of water in tissue. In general, tissue that is highly cellular or swollen have lower diffusion coefficient, thus helping in the characterisation of tumours. (differentiation, grading) [17]
source: [18]
DTI (Diffusion Tensor Imaging)
Diffusion Tensor Imaging (DTI) allows us to measure the connections in the brain, the directions and alignment of fibres by determining the diffusion of water molecules. This technique is an extension of Diffusion Weighed Imaging. It can be used to determine tumor type, heterogeneity, shape and size. [19]
Image source: [20]
Laboratory Tests
Evoked Potentials or EEG
Both these methods use electrodes placed on the patient's head and the measurement of the electric signals of the brain. They can also be used intra-operatively, to monitor the brain during tumour removal.
Image source:[23]
Biomarker Tests
Biological Markers indicate changes in tumour DNA. These tests can give information about tumour type, speed of growth, and help in treatment planning. These biomarkers can be retrieved from blood, plasma, CSF, urine, and saliva.[24]
Lumbar Puncture
A lumbar puncture in which cerebrospinal fluid, that surrounds and protects the brain and spinal cord, is harvested in tested. Tumour markers can be found in this liquid, in higher amounts than in blood, urine or spinal fluid.
Endocrine Evaluation
Hormone levels in blood and urine can indicate the existence of pituitary and hypothalamic tumours.[25]
Visual Field (Perimetry) Test
By assessing the visual field, information about the location of a tumour along the visual pathway can be determined. This test is performed by an ophthalmologist by flashing a series of lights into the patient's eyes and evaluating the response.[26]
Audiometry
This is a test in which an audiologist places headphones on the patient's head. Different tones in different sound ranges are directed into the ears of the patient, one ear at a time. This test can help determine whether a hearing loss is caused by tumours (nerve damage) or by eardrum/osccicle damage.[27]
DNA(Genetic) Profiling
DNA profiling, is a blood lab test used to determine the specific features of the patient's DNA,in order to develop the most suitable personalized treatments.
Biopsy
When a biopsy is performed,a small amount of tumour tissue is removed( during a surgery or as a separate procedure) and then sent for a pathological review .[28]
There are three kinds of brain tumour biopsy:
-Needle Biopsy: A hole is drilled in the skull, and then a hollow needle is inserted. Tumour tissue is removed from the core of the needle and sent for review.
-Stereotactic Biopsy: the same procedure as needle biopsy, but aided by computer-guiding systems in localisation and diagnosis
-Open Biopsy: the sample is taken during operation
Bibliography
[1] http://www.abta.org/brain-tumor-information/diagnosis/neurological-exam.html?print=t
[2] https://radiopaedia.org/articles/spin-echo-sequences
[3]http://cancergrace.org/lung/2007/04/18/xcytrin-for-nsclc-brain-mets/
[4]http://www.leedsneurosurgery.com/patients/brain_tumours/
[5]http://www.radiologyassistant.nl/en/p47f86aa182b3a/brain-tumor-systematic-approach.html
[6]https://www.radiologyinfo.org/en/info.cfm?pg=myelography
[7]https://www.radiologyinfo.org/en/info.cfm?pg=angiocerebral
[8]https://www.radiologyinfo.org/en/info.cfm?pg=angiomr
[9]http://www.ajnr.org/content/31/3/554
[10] https://en.wikipedia.org/wiki/Positron_emission_tomography
[11]http://www.snmmi.org/Patients/Disease_Condition/Content.aspx?ItemNumber=13312
[12]https://www.ncbi.nlm.nih.gov/pubmed/17161038
[13]http://radioactivityci2010.pbworks.com/w/page/32298574/fMRI
[14]http://www.medscape.org/viewarticle/776272_2
[15] https://radiopaedia.org/cases/glioma-mr-spectroscopy
[16]http://fmri.ucsd.edu/Research/whatisfmri.html
[17]https://radiopaedia.org/articles/diffusion-weighted-imaging-1
[18]https://www.slideshare.net/xanthoid/imaging-in-pediatric-brain-tumors
[19]http://link.springer.com/chapter/10.1007%2F978-1-4419-5858-7_2#page-1
[21]https://en.wikipedia.org/wiki/Magnetoencephalography
[22]http://www.massgeneral.org/psychiatry/research/neuroimaging_equipment.aspx
[23]http://www.olavkrigolson.com/that-neuroscience-guy/archives/04-2016
[24]https://www.thebraintumourcharity.org/understanding-brain-tumours/getting-a-diagnosis/biomarkers/
[25]http://www.abta.org/brain-tumor-information/diagnosis/laboratory-tests.html
[26]http://www.mayfieldclinic.com/PE-VisualFieldTest.HTM
[27]http://ucbraintumorcenter.com/acousticneuroma/audiogram/
[28]http://www.abta.org/brain-tumor-information/diagnosis/biopsy-procedure.html